Healthcare compliance isn’t slowing down, and 2026 is shaping up to be the year where multiple regulatory deadlines, new rules, and long-anticipated deadlines converge.
For healthcare organizations managing hundreds of contracts, this means one thing: Audit readiness is no longer just a compliance goal; it’s a contract management requirement. This guide breaks down what’s changing, how it impacts your contracts, and what teams need in place to stay fully audit-ready.
TL;DR What Healthcare Teams Should Expect in 2026
2026 will bring a combination of finalized rules and proposed updates that together will raise expectations around contract visibility, vendor oversight, standardized language, and fast access to documentation during audits.
Key developments include:
-
The proposed HIPAA Security Rule modernization
-
Finalized 42 CFR Part 2 alignment with HIPAA (compliance required by February 16, 2026)
-
New Centers for Medicare and Medicaid Services (CMS) Interoperability and Prior Authorization Timelines
-
Stricter scrutiny of BAAs and subcontractors, especially those handling SUD data.
For healthcare providers managing hundreds of Business Associate Agreements (BAAs) and PHI-related agreements, this means updated templates, tighter SLAs, centralized contract visibility, better version control, and contract workflows that make compliance provable, not just presumed.

As 2026 approaches, healthcare organizations face a complex mix of finalized rule changes and pending proposals that collectively elevate expectations for contract oversight. Even when a regulation is still in draft form, regulators increasingly expect organizations to demonstrate that they have processes capable of adapting quickly once rules become final.
For healthcare providers managing hundreds of Business Associate Agreements (BAAs), Protected Health Information (PHI)-handling agreements, utilization management vendor contracts, or Substance Use Disorder SUD)- related service agreements, this shift means that contract visibility and documentation readiness will be as important as the underlying compliance programs themselves.
A contract management system does not create compliance on its own. But it makes compliance repeatable, demonstrable, and easy to verify during audits—something regulators increasingly expect.
1. What Healthcare Regulations Are Changing in 2026?
2026 brings a mix of finalized rules and proposed updates that directly influence how healthcare organizations must handle BAAs, vendor agreements, PHI-handling contracts, and audit documentation.
Several major rules are fully finalized and carry firm compliance deadlines. Others are still proposed, but their direction is clear: regulators are pushing the industry toward stronger security expectations, faster interoperability, and more provable vendor oversight.
Why These Changes Matter for Contract Management
Even when a regulation is not yet finalized, regulators increasingly expect healthcare organizations to demonstrate that they can adapt quickly once rules take effect. The common theme across all 2026 changes is the demand for:
-
Greater contract visibility
-
Standardized, updated BAA language
-
Consistent vendor oversight
-
Detailed documentation that can be produced instantly during audits
-
Clear proof that PHI-handling vendors meet current expectations
For organizations managing hundreds of BAAs or vendor agreements, these shifts require contract workflows that are standardized, controlled, and easily verifiable.
Below is a breakdown of the developments most directly affecting contract language, BAAs, and audit workflows.
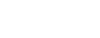
How will the Proposed HIPAA Security Rule Modernization Affect Contracts
The Department of Health & Human Services (HHS) has proposed major updates to modernize the HIPAA Security Rule to reflect the modern cyber threat landscape, particularly the rise in ransomware and targeted attacks against healthcare organizations.
If finalized as proposed, the HIPAA Security Rule Modernization will require organizations to strengthen cybersecurity safeguards and incorporate these expectations into BAAs and vendor contracts.
What the Proposed Rule includes:
-
Multi-factor authentication (MFA) across systems accessing ePHI
-
Encryption of PHI data at rest and in transit
-
Strongerengthened administrative safeguards
-
Enhanced cybersecurity preparedness documentation
-
Stronger expectations for vendor security proof and reporting
If finalized as written, organizations will need to update BAAs and vendor agreements to ensure these requirements cascade to every business associate touching BAAThis represents a shift from assuming security alignment to requiring explicit, traceable contractual compliance.
What Are the New Required or Expected BAA Clauses (Proposed)
BAAs will need updated language around redisclosure, subcontractor responsibilities, notification timelines, and any finalized HIPAA Security Rule requirements.
As regulations evolve, BAAs are becoming a primary focus for auditors. Many healthcare organizations still rely on outdated templates, leaving gaps that can cause audit findings.
Clarifying the 24-Hour Notification Requirement
Recent OCR proposals include new notification expectations and tighter oversight requirements. One area that often confuses is the 24-hour notification requirement. Here’s the accurate interpretation:
The 24-hour notice requirements apply to:
-
Activation of a contingency plan, and
-
Changes or termination of workforce access to ePHI
The 24-hour requirement does not replace
-
The 60-day breach notification timeline
Because this point is widely misunderstood, including explicit language in BAAs reduces audit friction and prevents misinterpretation during vendor oversight reviews.
Other expected BAA updates include:
-
Subcontractor flow-down obligations
-
Annual security and compliance attestations
-
Updated incident notification terminology
-
Aligning with any finalized Security Rule changes
-
Clear redisclosure restrictions for SUD data
What Is the Finalized HIPAA + 42 CFR Part 2 Alignment
The alignment of 42 CFR Part 2 with HIPAA requires organizations to update BAAs and Substance Use Disorder (SUD)-related contracts to include redisclosure restrictions, enhanced protections and new legal requirements by February 16, 2026
This alignment dramatically shifts how Substance Use Disorder (SUD) data is treated within healthcare operations with increasing penalties for improper disclosures.
❗Key impacts:
-
Patients may now sign a single consent permitting redisclosure for Treatment, Payment, and Operations (TPO).
-
Violations of Part 2 now carry HIPAA-equivalent civil and criminal penalties.
-
SUD records are prohibited from use in legal proceedings without a specific court order or patient consent.
-
Covered entities must update their Notice of Privacy Practices (NPP) by the compliance deadline.
-
BAAs must include redisclosure restrictions and flow-down obligations for SUD data.
🔎 What does Redisclosure Mean?
Redisclosure Definition:
Redisclosure occurs when a recipient of SUD-related PHI shares it again with another entity. 2026 rules require strict protections and clear language preventing unauthorized redisclosure.
This is not only a legal change. It directly affects the clauses in BAAs and SUD-related contracts.
RELATED READ: What Is Contract Management in Healthcare? (+5 Benefits)
Centers for Medicare and Medicaid Services (CMS) Interoperability & Prior Authorization Final Rule
This CMS rule sets firm requirements for payers, providers, and vendors across data sharing, prior authorization workflows, and FHIR API standards.
The CMS Interoperability & Prior Authorization Final Rule is designed to improve data sharing and reduce administrative delays in the healthcare system. These improvements come with strict timelines that must now be reflected in vendor agreements.
⏱️ Key deadlines:
-
Jan 1, 2026: USCDI v3 required for certain payers
-
Jan 1, 2026: Prior Authorization operational requirements begin
-
Jan 1, 2027: FHIR API Development (Patient Access, Provider Access, Payer-to-Payer, Prior Authorization APIs)
-
Ongoing: Information blocking penalties are enforceable
❗Contract implications:
Vendor agreements must include:
-
SLA updates that support the new prior authorization turnaround times (7 days standard, 72 hours expedited)
-
Indemnification language protecting the provider from vendor-caused CMS violations
-
Warranties guaranteeing FHIR API readiness
In short, vendor contracts must clearly commit to meeting API standards, turnaround times, and FHIR-based data exchange to keep providers compliant.
Increased Scrutiny on BAAs and PHI-Handling Vendors
Regulators are shifting from “do you have BAAs?” to “show me proof these BAAs reflect current requirements and that obligations are being performed.”

Auditors may request:
-
Current, up-to-date BAAs that reflect the latest regulatory changes
-
A complete inventory of PHI-handling vendors
-
Updated security documentation
-
Subcontractor lists and oversight evidence
-
Version histories showing when agreements were updated
-
Logs of obligations performed
-
Redisclosure limitations for SUD data in BAAs
-
API readiness or information-blocking compliance evidence (where applicable)
The shift is clear. Healthcare organizations are expected to demonstrate not only what their contracts say, but that the obligations inside those contracts are being performed
RELATED READ: 8 Best Practices to Make Contract Audits Faster, Easier, and More Cost-Effective
2. How Should Healthcare Organizations Prepare Contracts for 2026 Compliance
Preparing for 2026 is primarily about repeatable processes and provable documentation. Standardized contract language, version control, and evidence of vendor oversight are now table stakes for compliance teams.
A. Standardize Contract Language Across BAAs & Service Agreements
One of the biggest risks for 2026 is the presence of “orphan BAAs”—outdated templates that still get used, or that resurface during renewals.
Organizations should:
-
Use standardized templates with strict version control
-
Include updated clauses addressing PHI safeguards, redisclosure limits, subcontractor oversight, and notification requirements
-
Ensure all BAAs reflect 42 CFR Part 2 redisclosure protections if applicable
-
Update SLA timelines for interoperability or prior authorization vendors
-
Prevent old versions from being reused
Most regulatory changes include a transition period (typically 12 months after a rule’s effective date), but outdated BAAs become high-risk once that window closes.
Ensuring every team uses the correct, current version of your BAA template prevents “orphan BAAs” from resurfacing in high-risk areas.
Repositories should support metadata, versioning, and permissions out of the box.
B. Identify Contracts Requiring Update or Amendment
With so many contract versions in play, manual review becomes impossible. AI-assisted extraction and review helps identify:
-
PHI-handling vendors
-
Outdated BAA templates
-
Missing redisclosure restrictions
-
Missing subcontractor flow-down obligations
-
Agreements lacking MFA or encryption language (if needed once finalized)
-
Vendor contracts needing updated interoperability SLAs
This step also helps organizations build a searchable inventory of PHI-handling and SUD-handling vendors — something auditors are increasingly requesting.
C. Implement Renewal & Obligation Tracking
Auditors increasingly want evidence of performance, not just signed agreements.
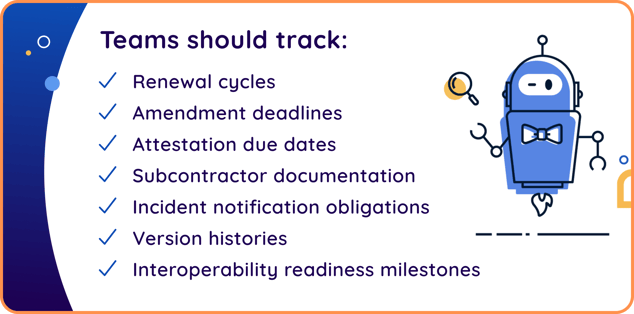
Teams should track:
-
Renewal cycles
-
Amendment deadlines
-
Attestation due dates
-
Subcontractor documentation
-
Incident notification obligations
-
Version histories for updated BAAs
-
Interoperability readiness milestones
Automated reminders help ensure nothing is missed. The goal is to show not just that obligations exist, but that they’re being actively monitored and completed.
What Compliance Auditors Look for in 2026
If the proposed HIPAA Security Rule is finalized as written, auditors may request evidence demonstrating:
-
Current BAAs with updated safeguards
-
PHI-handling vendor inventories
-
Documentation of subcontractor oversight
-
Logs of notifications, attestations, or verification activities
-
Version histories showing when updates were made
-
Redisclosure protections for SUD data (this is final and required)
Most auditors now prefer receiving information as structured “audit packets,” grouped by vendor, PHI status, and required documentation — a format that dramatically reduces back-and-forth.
Common Gaps That Cause Audit Failures
Frequent compliance issues include:
-
Missing PHI indicators
-
Outdated BAAs
-
Missing subcontractor documentation
-
Lack of redisclosure language for SUD data
-
Conflicting versions of BAAs across departments
-
Untracked auto-renewals
-
No documentation that obligations were performed
Nearly all of these failures map back to inconsistent templates, lack of visibility, or decentralized storage — which is why 2026 updates place such heavy emphasis on contract standardization.
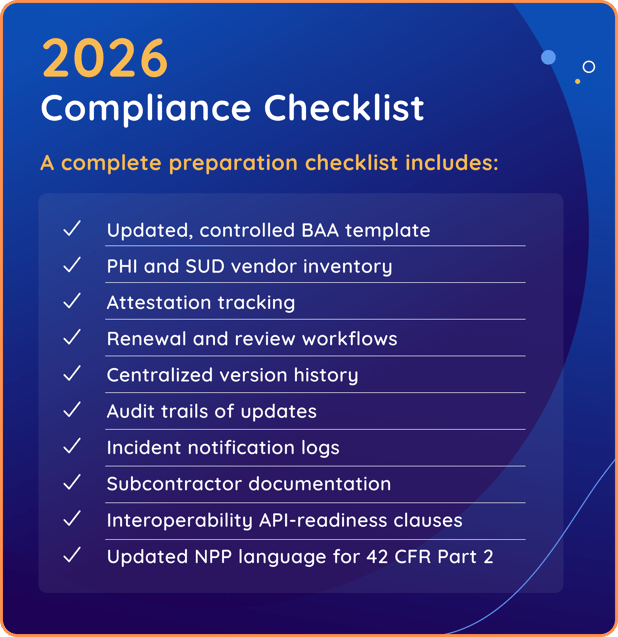
✅ 2026 Healthcare Compliance Checklist
A complete preparation checklist includes:
-
Updated, controlled BAA template
-
PHI and SUD vendor inventory
-
Attestation tracking
-
Renewal and review workflows
-
Centralized version history
-
Audit trails of updates
-
Incident notification logs
-
Subcontractor documentation
-
Interoperability API-readiness clauses
-
Updated NPP language for 42 CFR Part 2
RELATED READ: What Is Contract Compliance? 7 Best Practices To Ensure You’re Getting the Most Out of Your Contracts
3. Real-World Scenario: How a Mid-Sized Healthcare Provider Prepares for 2026
A mid-sized multi-site healthcare provider managing more than 300 BAAs, PHI-handling vendor agreements, and SUD-related contracts faces significant operational risk heading into 2026. Like many providers, their contracting process has evolved organically over time, resulting in scattered files, inconsistent BAA versions, and no reliable way to demonstrate compliance across dozens of PHI-handling vendors. As 2026 regulations approach, this fragmented system becomes a major operational risk.
🚧 Their challenges include:
-
BAAs are stored across inboxes, shared drives, and EHR attachments
-
Many BAAs are missing updated PHI indicators or 2026-required clauses
-
No unified inventory of PHI-handling vendors
-
No efficient way to generate documentation for upcoming audits
-
Renewal dates are tracked differently across departments
-
No evidence trail of vendor oversight or annual reviews
This provider knows that continuing with a decentralized approach is not sustainable. They need a contract system capable of surfacing gaps, enforcing version control, and making audit documentation easy rather than painful.
🌟 With ContractSafe, they’re able to:
Use AI Contract Review + Playbooks to:
-
Flag missing PHI indicators
-
Spot outdated or noncompliant clauses
-
Identify BAAs missing subcontractor flow-down or notification updates
Improve vendor oversight by:
-
Tagging all PHI-handling vendors and BAAs that require updates
-
Tracking annual vendor security attestations and subcontractor verification
-
Maintaining audit trails showing when agreements were reviewed or updated
Generate audit-ready documentation by:
- Producing audit packets in minutes, organized by vendor, PHI involvement, and required documents
Reduce risk across the contract lifecycle by:
-
Automating reminders for reviews, attestations, renewals, and updates
-
Maintaining a standardized, centrally controlled BAA template to prevent outdated versions from being used
With ContractSafe in place, this provider transforms the 2026 regulatory landscape from overwhelming to manageable.
What once took days or weeks — gathering BAAs, verifying versions, reconciling renewals, proving oversight — can now be executed reliably, consistently, and in minutes.
This makes the new 2026 requirements not just achievable, but operationally repeatable.
RELATED READ: Contract Management Challenges and How to Overcome Them
4. How ContractSafe Helps Healthcare Teams Stay Audit-Ready
ContractSafe gives healthcare organizations the structure, visibility, and audit-ready documentation needed to meet 2026’s elevated compliance expectations.
Together, these workflows create a consistent, defensible compliance process that supports BAAs, PHI-handling vendors, and audit preparation:
✅ Centralize & Organize All Healthcare Agreements
-
A secure, searchable repository for BAAs, service agreements, vendor contracts and SUD-related documents.
-
Role-based user permissions to restrict access to sensitive contracts
-
Version history that documents who changed what and when
-
Integration with Microsoft Word for seamless editing with audit trails
✅ Standardize Templates to Prevent Outdated Language
-
Store approved templates in one place
-
Ensure consistent language so teams aren’t editing ad hoc or reusing outdated versions
-
Easily update templates when regulations change
✅ Track Obligations, Renewals, and Vendor Compliance Activities
-
Renewal reminders keep reviews timely and prevent auto-renewals of outdated BAAs
-
Track annual vendor security attestations and subcontractor verification
-
Maintain a record of updates tied to regulatory changes
-
Automatically logs when requirements (attestations, reviews, subcontractor verification) are completed — creating the audit trail regulators want to see
✅ AI Contract Review to Flag Risk Before Auditors Do
-
Flag missing PHI indicators
-
Detects outdated or noncompliant clauses
-
Helps team review contracts at scale without manual line-by-line inspection
ContractSafe transforms scattered, inconsistent contract processes into a controlled, compliant system that helps healthcare organizations stay aligned with evolving 2026 regulatory requirements.
Key Takeaways
-
2026 brings a combination of finalized rules and proposed changes that together elevate expectations around contract control.
-
Contracts must reflect redisclosure limits, subcontractor oversight, API readiness, and potentially MFA/encryption requirements if proposed rules are finalized.
-
CMS Interoperability deadlines require tighter SLAs and stronger vendor accountability clauses.
-
Healthcare organizations must prepare not only BAAs, but also the proof that obligations are being performed.
-
Standardization and version control are essential to eliminate outdated BAAs.
-
A platform built for visibility and audit readiness—like ContractSafe—gives compliance teams the control and documentation they need.
As regulatory expectations rise, organizations that centralize contracts and enforce template control will be better positioned for fast, predictable audits.
A Forward-Looking Path to Compliance
By modernizing BAAs, improving visibility into PHI-handling vendors, and ensuring documentation is readily accessible, healthcare leaders can move from reactive compliance to proactive readiness.
Platforms like ContractSafe make this shift achievable by centralizing vendor agreements, enforcing template control, automating reminders, and providing audit-ready documentation without the complexity of a legacy CLM.
With a structured contract system in place, compliance stops being reactive — and becomes an operational advantage heading into 2026 and beyond.
Stop managing 2026 compliance with fear. Start managing it with proof.
👉 Request a Demo
FAQs
Are all 2026 Healthcare regulations final?
No. Some are finalized (e.g., 42 CFR Part 2 alignment, CMS Interoperability rules). Others—like the HIPAA Security Rule modernization—are still proposed.
Did the 24-hour notification requirement replace breach notification timelines?
No. Breach notifications remain subject to the 60-day requirement. The 24-hour notifications apply to contingency plan activations and access changes.
.
Do BAAs need specific language for SUD data?
Yes. 42 CFR Part 2 alignment is final and requires redisclosure restrictions and legal-use protections.
Will CMS Interoperability changes affect vendor contracts?
Yes. SLAs, indemnification clauses, and API-readiness warranties must align with the rule’s deadlines.
What are “audit packets”?
They are organized bundles of documentation—BAAs, attestations, subcontractor proof, version history—that auditors request during reviews.
How does ContractSafe help with compliance?
ContractSafe centralizes all agreements, enforces template control, tracks obligations, flags missing or outdated language, and makes it easy to produce documentation for audits.
Do we need a centralized contract repository to stay audit-ready?
Yes. Decentralized storage leads to outdated BAAs, missing redisclosure language, inconsistent versions, and gaps in vendor oversight. A centralized system makes it easy to maintain version control, track obligations, and produce audit-ready documentation in minutes.